Introduction
Like a chess champion planning their next move, a medical diagnosis is a complex process. It involves turns and twists that allow a physician to arrive at a conclusion. These turns and twists are a part of clinical diagnostics and they are areas that can be supported by Artificial Intelligence (AI). AI and medical diagnosis is challenging.
AI has a major role in the future of medical diagnosis. It’s not meant to replace physicians, just to augment the mechanism of healthcare delivery.
“The promise of artificial intelligence in medicine is to provide composite, panoramic views of individuals’ medical data; to improve decision making; to avoid errors such as misdiagnosis and unnecessary procedures; to help in the ordering and interpretation of appropriate tests; and to recommend treatment.” ― Eric Topol, Deep Medicine: How Artificial Intelligence Can Make Healthcare Human Again.
In this guide you will learn:
- What AI is and where it fits into the bigger picture.
- What the physician’s role in AI and medical diagnosis is.
- How AI can improve medical diagnostics.
- The main challenges with AI.
- How AI can directly impact business outcomes.
- Practical applications of AI in use and how they impact the mechanism of healthcare delivery.
- What’s in store for the future: AI in medicine.
What is AI? Where does it fit into the bigger picture?
AI is an overarching term that has many subcategories. AI IBM defines AI as any human-like intelligence exhibited by a computer, robot, or other machines.
AI is a part of our everyday life. A few common examples of AI in use today are speech recognition, natural language processing (NLP), image recognition, real-time recommendations, virus and spam prevention, automated stock trading, ride-share services, and autopilot technology.
The extensive reach of AI has been made possible due to the large amount of data available today, as well as computer systems that are capable of processing that data.
To start, we’ll define the following terms:
Artificial intelligence — anything that remotely resembles human intelligence.
Machine learning — a subset of AI applications. It learns by itself, adapts, takes in more data to perform a specific task with greater accuracy.
It’s already penetrated every industry including healthcare. It’s behind machines that are now making medical decisions based on images. Machine learning comes under the broader term of Artificial Intelligence. Machine learning gives computers the ability to learn without having to be programmed.
AI is growing rapidly and is used across different fields like education, finance, supply chain management, and, of course, healthcare. The IDC forecasts that spending on AI technology will grow to US 97.9 billion in 2023 - that’s 2.5 times the spending level of 2019.
Three subcategories of machine learning
Supervised learning — models are trained with labeled data sets. This allows the models to learn and grow more accurate over time.
Unsupervised learning — a program that looks for patterns in unlabeled data.
Reinforcement learning — trains machines through trial and error to take the best action by establishing a reward system.
Neural networks and deep learning are standard for any AI application. They can be defined as follows:
Neural networks — a class of algorithms that are modeled on the human brain where millions of processing nodes are interconnected and organized into layers.
Deep learning — machine learning but that uses deep neural networks with many layers. It has been widely adopted in the last decade, made possible by powerful GPUs (Graphics Processing Units).
What is the physician’s role in AI and medical diagnosis?
There is a fear that AI may replace physicians. It’s baseless. AI is meant to augment care and not to replace physicians. Currently, we are surrounded by systems that allow specific tasks to be done. The credit risk program in banks is one example of a system that is designed in this fashion. The credit risk program calculation may be hard for a human to do, but if you were to ask it to do a broader range of tasks, it would not be able to do these things at all.
How far are we until AI is on par with human intelligence? It’s hard to predict because we don’t really know. Twenty years seems to be an approximation and this has been stated for over 60 years. One area to focus on is machine learning, which is used in facial recognition programs and self-driving cars.
As technology develops, old jobs will disappear and new ones will come into the picture. I see an augmentation strategy here where humans and machines work together in an almost overlapping fashion. The landscape and work environment will change and healthcare providers will have to adapt.
There is great value in working with a network of physicians. It is important that they are active in the development process.
Aidence is a company that is working on AI-powered pathways for oncology. Their first AI clinical applications support automated medical image analysis for radiologists, specifically in early lung cancer detection.
According to Aidence, areas that need involvement from radiologists include…
- Before the development of the AI solution, physicians can help define the need for a clinically useful feature and a way to fit it into their workflow. If the aim is to improve their overall efficiency or provide highly accurate results to support their diagnostic decision, we must first understand how radiologists are currently working and what their reporting setup is. This understanding must also apply to diverse settings, varying per country and the type of hospital.
- During the development process, physicians may provide invaluable input for designing a user interface that is easy to use and complete.
- After deploying the AI product, the feedback channels must remain open. Real-world use can always enrich the research or test setting in which the product is built.
Studies have shown that deep learning is effective in diagnosing diseases.
Bias in AI may make things seem more rosy than they are. There are drawbacks to consider.
Diagnostic accuracy should follow an actual clinical setting. Applications that are designed based on actual clinical practice are important. While it’s good to compare datasets, it’s also important to compare diagnostic performance by comparing the dataset to people.
Accurate reporting is another limitation that should be considered. This is why knowledge and education and collaboration are paramount. By merging healthcare knowledge with technological expertise, successful reporting can be achieved.
Companies that are working on these problems should have access to clinical staff. Providers can offer a safety net in ensuring that diagnostics are as close to humans as possible.
How AI will improve medical diagnosis
The multitude of applications to treatment is noteworthy.
Disease detection: Deloitte performed an analysis on the various benefits of AI. Benefits ranged from enabling new business models to reducing headcount, improving productivity, creating new products, and enhancing existing ones.
The top benefit when it came to outcomes was the improvement of process efficiency. An example of this would be a process that is normally done by a human, like detecting patterns in a video.
Yet, there are novel approaches that are being deployed.
- Clinical decision-making process improvement.
- Treatment solutions can pick up the slack where we’ve fallen short in the past.
- Increasing life expectancy.
The main challenge. The big ‘Q’
The main challenge in adopting AI is quality, the big ‘Q’. Machine learning is really good at processing complex data. And this allows clinicians and researchers to discover new insights. Quality is paramount and beyond acceptance, the quality of data in the EHR will need to meet clinical standards.
Clinical registries are used for data collection. How will healthcare providers aggregate and process new streams of data? Translating AI to clinical value will largely be dependent on how data is collected and processed. It would be prudent to allow software companies to contribute their expertise. Software developers are working on solving all sorts of problems in the banking industry, manufacturing, agriculture and more. With the help of providers, the healthcare delivery mechanism will benefit from the same processes used in other areas of software development.
Transforming medicine and business outcomes
One of the issues that you may encounter is a lack of clearly defined outcomes for projects like this. Having use cases that are clearly defined will help with obtaining the outcomes that you would like to achieve.
While there are many applications of AI, here are a few that involve clinical and non-clinical applications:
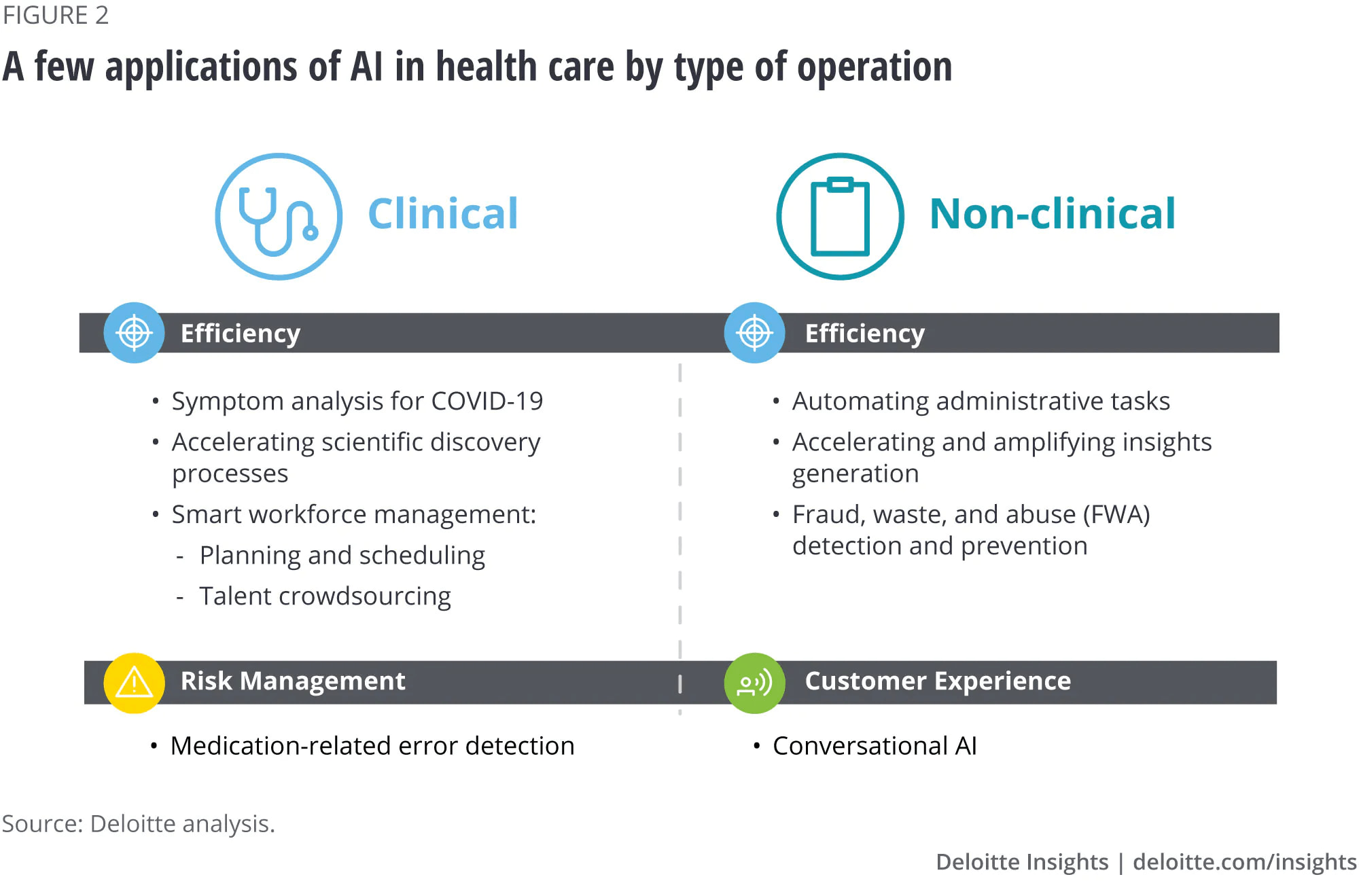
It’s important to start with our outcomes. Try walking back from what you are trying to achieve. Now that we have an idea of what the capabilities are, we can set parameters that will affect the outcomes.
The impact of AI will mean:
- Faster and more accurate detection of diseases.
- Automation data analysis, i.e., built-in classification systems.
- A decrease in unnecessary return visits.
- More objective and data-driven diagnostics.
Top applications — Practical applications and healthcare delivery transformation
Here are some examples of the top applications of AI. These companies have clearly defined use cases.
Capillary.io is a leading AI company working in the field of Rheumatology and it provides an all-in-one solution for capillaroscopy, (used to detect changes in the nailfold blood capillaries for diagnosis and follow-up of diseases such as scleroderma).
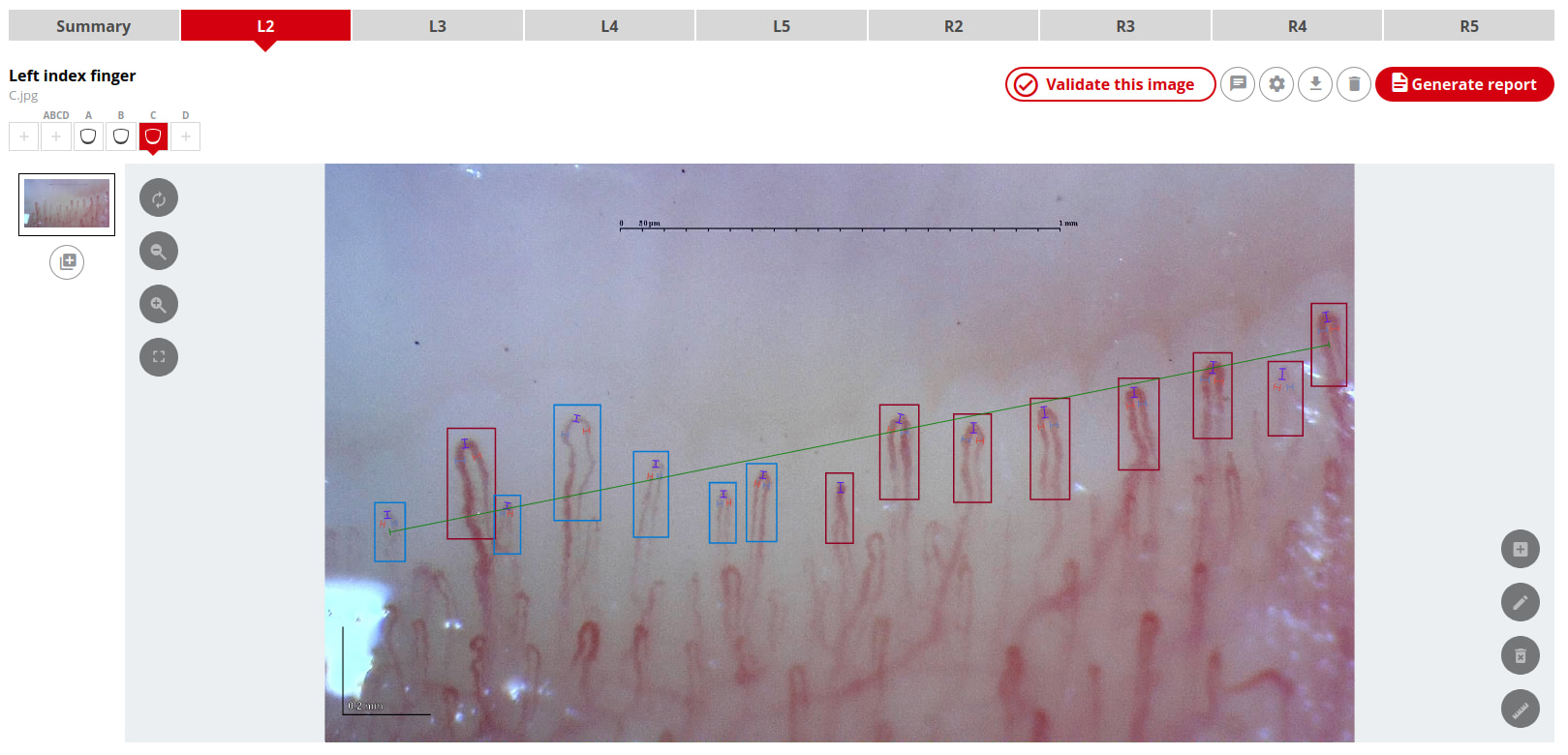
Veye Lung Nodules is an AI-based solution for pulmonary nodule management on chest CT scans. It detects, measures, classifies, and tracks the growth of pulmonary nodules as small as 3 mm. On default settings, Veye Lung Nodules detects nodules at a sensitivity of 90%. Aidence has received an AI in Health and Care Award to support the UK’s National Health Service (NHS) to reduce lung cancer mortality.

Savana is an international medical company that has developed a scientific methodology that applies Artificial Intelligence (AI) to unlock the full clinical value of free-text Electronic Health Records (EHRs), putting it in the hands of healthcare professionals to improve medical knowledge worldwide. With the world’s largest multicenter AI research network, the company generates tailored descriptive and predictive Deep Real World Evidence research studies to advance personalized, precision medicine. Savana is designed by physicians for physicians, maintaining the highest standards of privacy, offering projects in 5 languages: English, Spanish, French, German and Portuguese.
AI Augmented Healthcare is possible today
- Models will get better and better over time.
- Acceptance will increase and widespread adoption is a real possibility.
How to get started with your own program? A successful program begins with a solid data strategy:
Data → Machine Learning Model.
Data is the number one challenge with machine learning. Here are a few questions to ask when starting out on your next project:
- What data do we have access to?
- What data is not accessible, yet could be accessed if needed?
- What data is not available today, data that might be useful to us in the next 6-12 months?
- What is the bias in our data and/or sources of data?
How to know if you’re ready
Define your business problem. Could it be solved using machine learning? What are the metrics for success? Not every problem is solvable by machine learning. If you take a see what sticks approach, you may end up wasting resources.
Stakeholders should be available and behind the effort. It’s also good to have the technical team available so that people are working in a coordinated fashion.
There can be a lot of technical know-how involved when setting something like this up. Take advantage of existing tools that can help. The companies previously mentioned have done the heavy lifting. Workflows that pertain to the work being done streamline your work, allowing you to focus on being where you add the greatest value.
Here are some ideas on answering clinical needs with AI solutions
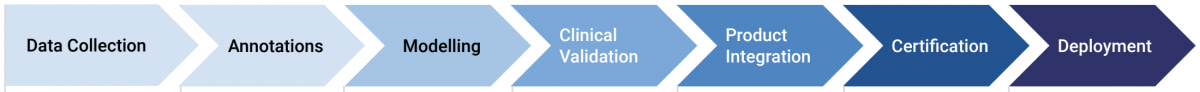
- Data collection - AI lives off data and relies on fundamental scientific principles. We gather large numbers of high-quality datasets from diverse modalities, hospitals, and countries, and anonymize studies to process them in line with GDPR.
- Annotations - Radiologists must annotate the obtained scans to ‘teach’ the AI model; for high accuracy, multiple readers are preferred for each scan.
- Modelling - This stage comprises the training of the model and defining the outcome of the algorithm based on recommendations from medical societies and input from radiologists.
- Clinical validation - The performance of an AI model is validated on a test set. This dataset is independent of the one used to train the algorithm and contains the ground truth – the radiologists’ final assessment. To advance research, the results of the validation are made public.
- Product integration - We integrate our tools into the radiologists’ pre-existing workflow and IT infrastructure.
- Certification - The technical documentation containing the clinical evaluation report and the risk assessment for the device is submitted to a notified body (i.e., an organization designated to assess the conformity of certain products before market release).
- Deployment - Deploying the AI solution in clinical practice means site integration, piloting, and testing. The process does not end with deployment – engineering and service are as important to maintain the quality of the solution. User feedback and a solid Post-Market Surveillance plan are how we can keep improving.
Outcomes. Plan for the long term. With a system like this in place, you’ll easily be able to grow. Data is managed for you, which is something that is missing in many healthcare organizations and practices.
Conclusion
AI and medical diagnosis is a new frontier. With the recent world events, approaches that have been previously discussed will accelerate into mainstream healthcare. By getting the right support, you can succeed while taking advantage of what is now available. AI projects take planning just like any other implementation.
Tip: If you want to learn about how our tool can help you save time, and resources while evaluating Rheumatology patients using Nailfold Capillaroscopy, feel free to contact us here.
Victor Phillips is a physician, healthtech writer and business consultant. Contact him for help with your next project.